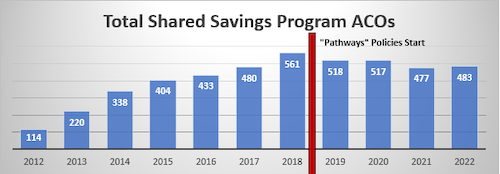
January 27, 2022 – The number of accountable care organizations (ACOs) in the Medicare Shared Savings Program (MSSP), the country’s dominant value-based payment program, only modestly increased to 483 in 2022. Following multiple years of flat or declining ACO growth, today’s announcement is disappointing and should send a wake-up call to an administration whose goal is to have all traditional Medicare patients in an accountable care model by 2030. There are still fewer patients in ACOs and ACOs in the program than there were in 2020.
There are 46 ACOs starting their first initial agreement period this year, but of these many have previous experience in Medicare ACO programs, including the now-expired Next Generation ACO Model. The MSSP hasn’t rebounded from where ACO participation was before CMS’s 2018 rulemaking, dubbed “Pathways to Success,” that forced more ACOs into risk. Following a high of 561 MSSP ACOs in 2018, participation fell the next two years and to 477 in 2021. Last year, the CMS Innovation Center set a goal to have all traditional Medicare beneficiaries in a care relationship with a provider who is accountable for their quality and total cost of care by 2030. That includes ACOs, and while it’s a lofty goal, it’s one NAACOS strongly supports, but it won’t get there with just wishful thinking. Action is needed to increase participation in ACOs.
NAACOS has offered several suggestions to attract new ACOs while retaining existing ones, including increasing ACO shared savings rates, fixing key benchmarking and risk adjustment issues, allowing more time before requiring risk, minimizing administrative burdens, rethinking quality reporting requirements, and providing more timely and complete data.
