PDPM may bring about some subtle changes in care management.
 Medicare’s new payment system for post-acute-care facilities – the Patient Driven Payment Model, or PDPM – will bring changes to SNFs’ accounting and coding departments. It will also encourage SNFs to take a more individualized approach to the care of each resident, and it will reward them for doing so.
Medicare’s new payment system for post-acute-care facilities – the Patient Driven Payment Model, or PDPM – will bring changes to SNFs’ accounting and coding departments. It will also encourage SNFs to take a more individualized approach to the care of each resident, and it will reward them for doing so.
“PDPM is a reimbursement change, not a clinical change, for our facilities,” says Nate Ovenden, RAC-CT, senior Medicare & managed care consultant, Good Samaritan Society, Sioux Falls, South Dakota. “I don’t see it directly impacting any incontinence issues we see in our buildings. What is medically necessary in RUGS IV is still medically necessary under PDPM. That is something CMS has been very clear about, and they will monitor drastic changes in behavior from RUGS-IV to PDPM.
“Our facilities have been trained to do the right thing at the right time for the right person,” he continues. “The only difference is that PDPM will help offset the costs of doing so a little more than RUGS-IV. So there is a bit of light at the end of the tunnel for facilities that have been doing the right thing.”
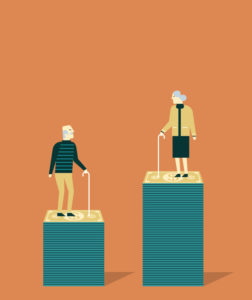
Winners and losers
Effective Oct. 1, PDPM is designed to be budget-neutral. But there will be winners and losers.
The winners? Skilled nursing facilities that accurately assess the needs of the resident upon admission, and provide care accordingly.
The losers? Facilities that cling to the old reimbursement method, which rewards SNFs that maximize the number of hours they spend providing physical therapy, occupational therapy or speech/language pathology therapy. Under PDPM, more therapy hours won’t add up to more reimbursement dollars. (That said, the level of therapy anticipated for each resident will continue to be one factor in the new reimbursement scheme.)
Under PDPM, residents will be classified into one group for each of five case-mix-adjusted components:
- Physical therapy (PT).
- Occupational therapy (OT).
- Speech/language pathology (SLP).
- Nontherapy ancillary services (NTA).
For each of the components, there are a number of groups to which a resident may be assigned, based on the relevant MDS 3.0 (assessment) data. There are 16 PT groups, 16 OT groups, 12 SLP (speech/language pathology) groups, six NTA groups, and 25 nursing groups. PDPM classifies residents into a separate group for each of the components, which have their own associated case-mix indexes and per diem rates. Additionally, PDPM applies per diem payment adjustments to three components, – PT, OT, and NTA – to account for changes in resource use over a stay. The adjusted are then added together (with the unadjusted SLP and nursing component rates and the non-case-mix component) to determine the full per diem rate for a given resident.
Dollar impact
PDPM’s impact on incontinence care will depend not only on the component case-mix payment rates, including Minimum Data Set (MDS) resident assessment items that are clearly incontinence-related, says Dan Ciolek, associate vice president, therapy advocacy, American Health Care Association. “It also depends on other MDS items that can be influenced by or are side effects of incontinence issues.”
For example, the non-therapy ancillary (NTA) component assigns points to specific services and conditions associated with higher NTA costs, Ciolek explains. Three incontinence-related MDS items (H0100C – Appliances: Ostomy; H0100D – Appliances: Intermittent Catherization; and I1300 Ulcerative Colitis, Crohn’s Disease, or Inflammatory Bowel Disease) are each assigned one NTA component point.
“Depending on how many of these are present and other conditions and treatments identified on the MDS, these incontinence-related MDS items may impact PDPM rates from roughly $20 to $50 per day,” he says.
In the nursing component, MDS items H0200C and H0500 – denoting urinary and bowel toileting training programs, respectively – are used as case-mix rate adjustors for eight of the 25 PDPM nursing component groups. They may impact PDPM rates from roughly $5 to $25 per day if associated restorative nursing services are also furnished, says Ciolek.
Incontinence issues often are directly associated with infections, skin conditions (including decubitus ulcers), functional impairment, falls, and cognitive impairment associated with disturbed sleep patterns, he continues. These factors can significantly impact the PDPM case-mix groups for the NTA and nursing components, as well as impact the physical therapy, occupational therapy, and speech-language pathology PDPM components.
(Repertoire readers should note that for the first three days of the stay, providers will receive 300 percent of the calculated NTA payment component, to account for the typically heavy investment in med/surg supplies, drugs. etc., at the beginning of a resident’s stay. Starting on Day 4, this will drop to 100 percent.)
Subtle changes
PDPM may bring about some subtle changes. Because PDPM is meant to be more patient-centered, nursing must ensure that caregivers accurately and fully describe the impact of the patient’s continence status, as that will be associated with the cost of pull-ons, incontinence pads or adult briefs,” says Dea J. Kent DNP, RN, NP-C, CWOCN, president-elect, Wound, Ostomy and Continence Nurses Society™ (WOCN®).
“Incontinence, whether bowel or urinary, is a valid diagnosis that requires a medical supply,” she continues. “Currently, incontinence supplies in some facilities may be accounted for, or may be billed, to the patient. It will be interesting to see how this model operates upon implementation. Some components of incontinence care go unaccounted for, such as preventative creams, which ensure that skin health is maintained in areas that incontinence may affect. No single category in the current or future payment model accounts for those costs.”
Instead of the traditional “one-size-fits-most-everyone” approach, long-term-care providers will have to be thoughtful about what stock they carry, versus what individualized items they carry, she says.
“I hope that gone will be the days that because there is only one size of adult brief available, everyone who is incontinent will have that size placed on,” she says. “That is not the most dignified approach, it is not evidence-based, and it certainly does not support the Triple Aim,” that is, improving the patient experience of care, improving the health of populations, and reducing the per capita cost of healthcare. “In fact these practices actually lead to more urinary dependency,” she says.
“I also hope that it becomes standard practice to thoughtfully promote continence behaviors, even in the memory-impaired patient. Toileting is cheaper than placing a brief, and is less cumbersome on the staff. A focus on prevention of moisture-associated skin damage may also mean less pressure injury/ulcer development, since the skin health in those moist areas may have a hyperfocus instead of being an afterthought.
“Lastly, more continence awareness may lead to better assessment, and better and more appropriate intervention, which ultimately will make less work for caregivers, allowing them to spend more quality time with their patients.”
The need for facilities to help residents with bladder or bowel issues for quality and to maintain dignity will affect the products they select, says Susan LaGrange, RN, BSN, NHA, CDONA, FACDONA, CIMT, IP-BC, director of education for Pathway Health in Lake Elmo, Minnesota. For example, the old incontinence brief may be OK for more dependent people, but there are many products designed for younger and more independent residents in the future, she says. It is essential to assess residents for the type of incontinence and to plan an appropriate program.
Because restorative nursing calls for providers to help residents achieve their highest level of functioning, it’s no surprise that things that aid mobility – e.g., canes and walkers – will be on their shopping list as well, just as adaptive equipment for eating has proven effective for some patients who were unable to feed themselves, she adds.
For suppliers, “the theme of the day is ‘value,’” says Ciolek. “Providers are going to become more sensitive to the balance between the overall costs of the incontinence-related products/devices/equipment, and their effectiveness. Once a person becomes incontinent, the costs of care and risks for additional negative health consequences increase markedly, so savvy providers will most likely be seeking solutions that would be effective at helping prevent or reverse incontinence.
“For residents whose incontinence is unlikely to be reversible, knowledgeable providers will be seeking solutions to reduce the risk for secondary health and psychological complications as well as avoid or minimize increases in direct staff care time needed to use the incontinence-related products/devices/equipment.”
Editor’s note: The Wound, Ostomy Continence Nurses Society has an online algorithm to assist caregivers with incontinence product implementation. It can be found at bwap.wocn.org.
The ‘highest level of functioning’
Restorative nursing for incontinent residents
The concept of “restorative nursing” will play a strong role in incontinence care at post-acute-care facilities under PDPM, as it has under RUGS-IV, says Susan LaGrange, RN, BSN, NHA, CDONA, FACDONA, CIMT, IP-BC, director of education for Pathway Health in Lake Elmo, Minnesota.
The concept has existed for years, says LaGrange, who teaches restorative nursing around the country. It’s a formal program based on resident assessment that works on specific restorative programs, for example, passive range of motion, active range, splint or brace, bed mobility, walking, transfer, dressing, grooming, eating and swallowing, amputation or prostheses care, communication and toileting, she says.
“The whole idea is to keep residents at their highest level of functioning,” she says. What’s more, particularly for toileting, it’s a matter of maintaining residents’ dignity.
Evaluating a resident’s need for incontinence care calls for an interdisciplinary team approach. Not only does the facility have to consider the resident’s toileting patterns, but other components that might be relevant, such as the person’s cognitive abilities, diagnosis, medications, and ability to get up and go to the toilet. The team also must identify the type of incontinence they’re dealing with. Someone with stress incontinence – that is, a resident who experiences small to moderate leakage when laughing or coughing – will have different needs than someone who is incontinent because they can’t get out of their chair or bed in time to get to the toilet.
When attempting to determine the type of incontinence, bladder scanners are a much less invasive way than catheters to identify how much urine the resident is retaining post void, she says.
“Depending on all these different types – the care plan will be different,” says LaGrange, In the past several years, facilities have begun to focus on fecal incontinence as well as urinary, she adds.
Begin at the beginning
Traditionally, restorative nursing has often commenced only after formal therapy was completed in the long-term-care setting, points out Dea J. Kent DNP, RN, NP-C, CWOCN, president-elect, Wound, Ostomy and Continence Nurses Society™ (WOCN®). But under PDPM, facilities would be well-advised to evaluate residents and coordinate restorative nursing with therapy at the beginning of the stay. If they fail to indentify the need for restorative therapy upon admission, they won’t be able to capture reimbursement for it unless they undergo an interim payment assessment, or IPA.
“In order to achieve the most success with patient care and the changing payment model, I believe the savvy director of nursing will partner with both the staff educator and a continence expert, such as a Certified Wound Ostomy Continence Nurse from the community at large, to provide education, empowerment and validation for licensed and non-licensed nursing staff alike regarding incontinence etiology, treatment, containment, recognition and prevention.
“It will be important to recognize not just the type of incontinence from a medical pathology standpoint, but to also recognize the level of incontinence. The level of incontinence and type, in combination with mobility status, can be utilized to implement evidence-based best practice for appropriate product utilization as well as sound skin breakdown prevention strategies.
“This up-front education and validation will definitely allow the staff to provide timely, accurate and effective management of incontinence, which should not only contain and streamline costs, but likely promote an increase of quality of care, while maintaining and even boosting the self-image of the patients who are living with incontinence of all types.
“Additionally, bowel and bladder programs have been mandated for years, and at this point, the importance of restorative nursing care will exponentially increase.,” she says. “The demand for restorative nurse aides to assist with bowel and bladder programs to promote continence must have a serious renaissance.”
Incontinence: Not necessarily a forever thing
Incontinence impacts many short- and long-stay residents in a nursing facility, says Dan Ciolek, associate vice president, therapy advocacy, at the American Health Care Association. “Not only are there numerous physical-health-related consequences, but residents can also be psychologically impacted by a loss of dignity and could become susceptible to social isolation and depression.”
PDPM’s emphasis on individualized care, along with new quality standards, may help.
Many forms of incontinence are preventable, and some can be reversed with focused interdisciplinary approaches, says Ciolek. The implementation of PDPM will align payments with the SNF Requirements of Participation (RoP) and Quality Reporting Program (QRP), he points out. “This creates opportunities for providers to explore and develop innovative solutions to reduce the costs of care while maintaining or improving quality. I believe that over the next few years, providers will be exploring ways to prevent and treat incontinence using evidence and best practices.
“I have seen examples where SNFs have developed incontinence risk assessments, monitored the prevalence of incontinence, monitored call light patterns, conducted staff time studies, evaluated falls with and without injuries, noted prevalence of urinary tract infections and hospitalizations, identified associated skin disorders, tracked functional independence, and evaluated resident, family and staff satisfaction and laundry and supply costs associated with residents at-risk for or who are currently incontinent,” he continues.
“From these analyses, they changed practices and interventions to be more evidence-based and resident-centered. For example, in states whose laws permit it, SNFs are identifying residents that are clinically appropriate for the delivery of Percutaneous Tibial Neuromodulation (PTNM) within the scope of practice of physical therapist services for certain types of urinary incontinence. They are experiencing notable improvements in the quality of care and resident and employee satisfaction, while reducing overall costs.”
