Sponsored by McKesson Medical-Surgical
Your outpatient labs need you.
As a supply chain executive, you may not be conversant with hematology, chemistry, immunoassays, analyzers, molecular testing, point-of-care testing or CLIA. You may not be familiar with the supply-chain-related demands of the typical outpatient lab.
And yet, chances are, your health system has been actively acquiring physician practices, surgery centers, urgent care centers, even retail clinics, over the past few years. And with each one comes a lab.
“Having lab testing close to the point of the patient encounter with immediate results, diagnosis and treatment in the non-acute space of the health system can be an essential component in achieving higher quality outcomes and increased patient satisfaction,” says Lynn Glass, Vice President of Strategic Accounts, Lab, McKesson Medical-Surgical. ”Failure to fully integrate a lab strategy that addresses standardization, upgrade in product, and efficiencies impacts both supply chain and patient care with decreased operational and financial efficiencies and delayed care to patients with lower quality outcomes. Having a distribution partner who understands the complexities encountered with acquisition and consolidation and the benefit of an integrated lab strategy is essential to healthcare delivery in today’s environment.
A key pillar
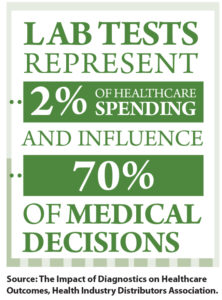
“Laboratory is a key pillar to success with value-based-care programs from government and private payers alike,” says Patrick Bowman, Director, Strategic Accounts, Lab, McKesson Medical-Surgical. “A significant amount of a health system’s revenue is based upon value-based-care programs, which essentially score an organization’s ability to achieve certain benchmarks, many of which require both a higher level of patient compliance and completed laboratory results.”
Lack of control over those labs can have negative operational, financial and clinical consequences.
“Having multiple laboratory products that execute the same function can result in clinical inefficiencies, as not all tests replicate the same result and range,” he says. “This leads to both confusion and potential misdiagnosis. Purchasing efficiencies are also sacrificed, as without a strong formulary, the opportunity to negotiate for best price tier from the distributor or manufacturer may be missed.”
Glass adds, “As health systems acquire more and more sites, things can become increasingly disorganized. There may be no standardization of products or processes. You might find a hundred non-acute locations, each one ordering from a different vendor, ordering different tests, and employing different supply chain processes.”
Health system administrators – including supply chain executives – might assume (or hope?) all those non-acute operations are taking care of themselves, Glass says. “And they are … but they might not be doing a very good job of it.”
Point of care
 Some healthcare systems opt to pull all testing out of the non-acute clinics and into a central lab, says Bowman. “I think the easy answer for many is, ‘We have this hospital lab that runs like a well-oiled machine, so we can do our tests there at a fraction of the cost.’”
Some healthcare systems opt to pull all testing out of the non-acute clinics and into a central lab, says Bowman. “I think the easy answer for many is, ‘We have this hospital lab that runs like a well-oiled machine, so we can do our tests there at a fraction of the cost.’”
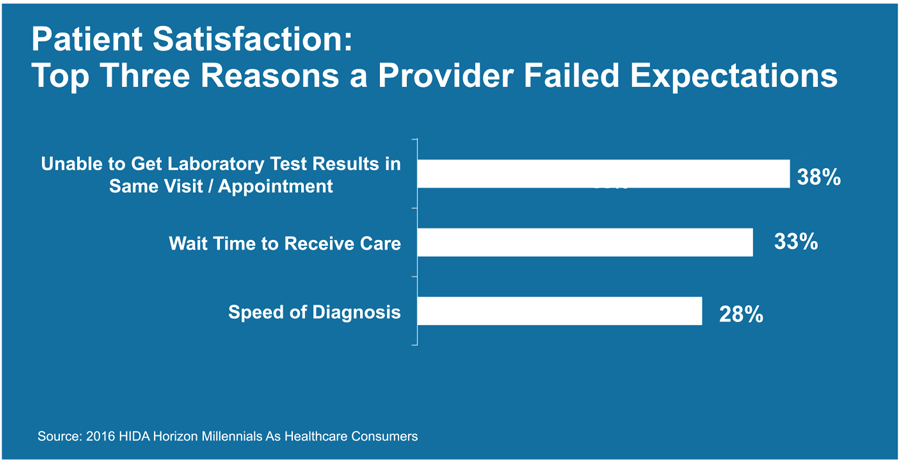
But doing so can lead to unacceptable delays getting results, making a diagnosis, and beginning treatment, he says. What’s more, a high percentage of patients – particularly those with chronic conditions – fail to comply with instructions to go to a central lab for a test. That’s a problem, because patient compliance and engagement are in direct correlation with better patient outcomes.
“It’s important to see the big picture, to have a strategy,” he says. “Keep as close to the clinicians as possible those tests whose results are needed quickly,” even if the nominal cost of running them at the central lab might be less.
“It’s important to address and provide healthcare in conjunction with value-based care,” adds Glass. Utilizing point-of-care lab testing provides immediate diagnosis, treatment and a higher quality of care. This will impact both reimbursement and the overall patient experience, and also addresses management of the chronic disease patient population.
Supply chain’s role
Just as they must in the hospital, supply chain executives must work as part of a team to take control of the scattered non-acute labs.
“Decisions on non-acute lab strategy should be made by committee, which will often include representation from nursing staff, medical leadership, supply chain, finance and the laboratory director or manager,” says Bowman. “A committee of this size and scope is essential, because non-acute laboratory testing can greatly impact each of their respective areas of responsibility.”
A distributor with experience in the non-acute lab setting can help the team make sound decisions. For example, McKesson can help supply chain executives take control of the non-acute continuum through improved supply chain operations, stronger financial performance and building a clinical infrastructure that leads to better outcomes.
“A large hospital lab operates very differently than lab in the non-acute space of a health system,” says Glass. “A distributor with the capability of servicing the large hospital may not have the same level of expertise in the non-acute sites. Adds Bowman, “The delivery model is key in this space. An acute hospital lab is likely to have semi-trucks backing up to their dock and delivering supplies once a week. But the larger system might have 50 to 100 sites with ongoing needs for point-of-care lab supplies. They need a vendor that can deliver in vans to all those sites, and who knows how to pack and ship in small quantities, while maintaining product integrity throughout the chain.”
 McKesson supply chain operations has a storage and delivery model that can efficiently provide cold chain storage and delivery, lot track and trace, lot sequestration and shipments in low units of measure, and additionally has relationships with prime vendors to afford best contracting and pricing. McKesson can sequester specific lots of reagents, supplies and controls, then deliver them to the non-acute sites as space allows.
McKesson supply chain operations has a storage and delivery model that can efficiently provide cold chain storage and delivery, lot track and trace, lot sequestration and shipments in low units of measure, and additionally has relationships with prime vendors to afford best contracting and pricing. McKesson can sequester specific lots of reagents, supplies and controls, then deliver them to the non-acute sites as space allows.
“We’re more than a distributor,” says Glass. The company’s strategic account teams, point-of-care specialists, lab equipment specialists, consultants and technology resources can help health systems implement solutions that drive increased revenues, operational and financial efficiency, and a higher quality of care to the patient with better clinical outcomes and higher patient satisfaction.
“It’s a matter of changing the conversation, changing the whole process by which lab services are provided and collaborating to determine a new strategy that best serves their patients and provides the highest quality in lab testing.”