Provider, manufacturer, and distributor numbers to consider for your supply chain strategy.
By John Strong, Co-founder, Access Strategy Partners Inc

With all the data out there, Frontiers© wants you to stop and ponder a few numbers we unearthed in the past couple of months.

Smart orthopedic implants are on the horizon, and at a cost estimated at $20,000 each.1 In fact, CMS has already aligned certain incentives for monitoring a patient’s joint replacement procedure to reimbursement. Developers say these are a sure-fire way to help improve outcomes. How will you evaluate this technology? The same article notes that the number of total knee replacements will grow from 1.4 million in 2025 to 3.4 million in 2040.
A January 2015 Forbes survey indicated that 24% of medical device manufacturers reported the biggest challenge in their business was “managing geopolitical risk.”2 We would argue that with rising tensions with China and Russia, that number is already growing exponentially in 2022. Healthcare providers need to seriously consider this risk with regard to their procurement strategies this year. In fact, the value of U.S. imports from China for pharmaceuticals and medical equipment, products and supplies reached $20.74 billion in 2019.3 Our foreign relations issues include “supply chain disruption and (reduced) manufacturing capacity,” according to Paul Keckley.4 How dependent is your supply chain on Chinese-made ingredients and finished goods?
As of January 2022, between 8,000 and 12,000 containers containing medical supplies were being held up at U.S. ports. While we hope at press time the number will be lower, the fact is that this has caused shortages of commonly used, relatively inexpensive medical products that has driven prices higher. For example, there are currently plenty of aluminum crutches available at $40 per pair, but none at current contract prices of around $14 per pair.5 Is your sourcing strategy pivoting to the new realities of supply and demand beyond price alone? Are you considering the carbon-footprint of these cheap supplies or willing to pay more for U.S. made products?
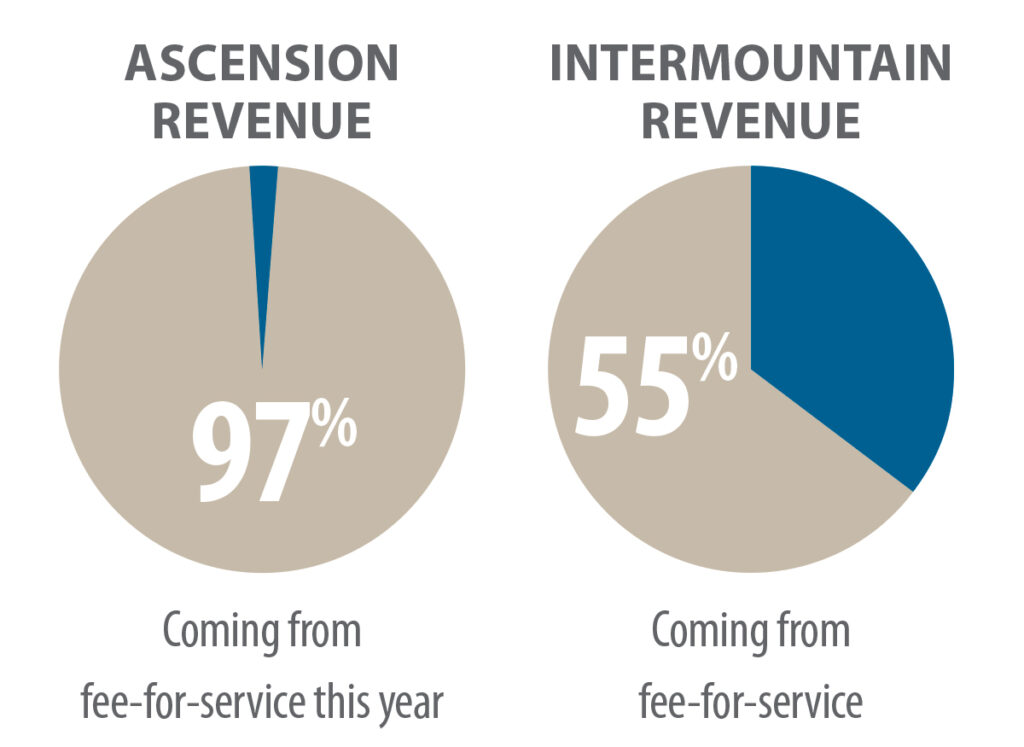
Value-based contracting was on full display at the J.P. Morgan Health Care Conference earlier this year. It showed clearly that the rate of adoption of VBC is unbalanced across the industry, but that it continues to grow. It was reported that 97% of Ascension revenue was still coming from fee-for-service this year, while 55% of Intermountain revenue will be coming from fee-for-service. How is the transition to value-based contracting going to affect your supply chain and contracting strategies moving forward over the next three to five years?
Are you buying for, or selling to “payviders?” More and more hospitals are entering into commercial employer-based risk contracts, as well as Medicare and Medicaid programs, according to the Healthcare Financial Management Association. As providers do this, we expect more value analysis emphasis placed on product value (not price) that can reduce readmissions and improve patient outcomes the first time a procedure is performed. Is your supply chain and value analysis committee ready to research and uncover the facts around how products under consideration actually perform? Can suppliers provide assistance with this?

According to a December 2021 press release, almost 80% of hospital leaders say supply chain optimization reduces costs and improves margins.6 It goes on to say that implementing more efficiencies and identifying certain waste(s) in the supply chain can reduce hospital expenses by 17.7% per year. On the other hand, a report by Accenture in early autumn of last year showed that only 38% of supply chain executives feel that their staff is “mostly or completely” ready to leverage the technology tools provided to them. How are you training your staff to use the technology you already have, much less new technology? Are you growing weary of “We have an app for that?”
According to “Supply Chain Dive,” there are five product classes that will be in short supply in 2027. While none of these are a surprise to you, they deserve consideration among your sourcing specialists.
- No. 1: Semiconductors. How will that impact your new equipment and replacement purchases in 2022?
- No. 2: Aluminum. Will we be back to wooden crutches? Can we? Some readers probably don’t even remember them.
- No. 3: Food products. Are your food brands free of COVID-based production and transportation problems? Are they imported?
- No. 4: Plastics. Uh-oh! We use lots of plastic in healthcare. If Starbucks® cannot source enough plastic cups, can you? At what price? Where does our resin come from?
- No. 5: Building materials. Overall construction input prices are up about 22% over a year ago. Can we put the brakes on that new building or remodeling?
Is private equity sniffing around your organization? Private equity healthcare deals increased from $41.5 billion in 2010 to almost $120 billion in 2019, according to a white paper from the University of California-Berkeley and the American Antitrust Institute.8 How would PE investors view your present supply chain?
1 Cohen, Jessica Kim, “Implants get ‘smart’ in orthopedics”, “Modern Healthcare”, December 6, 2021, pp 2729, 37-40.
2 Stirling, Chris and Shehata, Ash, “Collaboration—The future of innovation for the medical device industry” © 2016 by KPMG International.
3 Statistica, © 2022.
4 Keckley, Paul, “Two Events this Week will Set the Tone for the Rest of 2022 in U. S. Healthcare”, “Keckley Report”, February 7, 2022.
5 JHC research, December 2021.
6 © 2022 by Siftco.
7 Zimmerman Sarah, Supply Chain Dive, “Shortages 2022: 5 products expected to be in tight supply this year”, January 31, 2022.
8 Kacik, Alex at “Modern Healthcare.com”. “Corporate investors reshape healthcare industry”, December 18, 2021.
