As the population ages, the risk for falls rises
 Falls are the leading cause of injury-related deaths among persons aged 65 and over, and the age-adjusted rate of deaths from falls is increasing. The Centers for Disease Control and Prevention released its most recent statistics this spring.
Falls are the leading cause of injury-related deaths among persons aged 65 and over, and the age-adjusted rate of deaths from falls is increasing. The Centers for Disease Control and Prevention released its most recent statistics this spring.
Advanced age is an independent risk factor for falls. But so are related factors such as reduced activity; chronic conditions, including arthritis, neurologic disease, and incontinence; increased use of prescription medications, which might act synergistically on the central nervous system; and age-related changes in gait and balance.
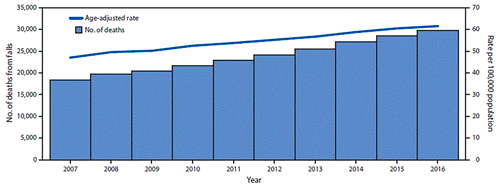
Approximately one in four U.S. residents aged 65 years or older report falling each year, and fall-related emergency department visits are estimated at approximately 3 million per year, according to the CDC. In 2016, a total of 29,668 U.S. residents aged 65 and over died as the result of a fall (age-adjusted rate of 61.6 per 100,000), compared with 18,334 deaths (47 per 100,000) in 2007.
The rate of deaths from falls among persons aged =65 years increased 31 percent from 2007 to 2016, increasing in 30 states and the District of Columbia, and among men and women. Among states in 2016, rates ranged from 24.4 per 100,000 (Alabama) to 142.7 (Wisconsin). The fastest-growing rate was among persons aged =85 years (3.9 percent per year).
In 2016, there was a higher rate of fatal falls among older men, in contrast to the rate of nonfatal falls, which is higher among older women. This might have resulted from differences in the circumstance of a fall (e.g., from a ladder or while drinking), leading to more serious injuries, including head trauma, or higher rates of postfall complications in men.
Adults aged =85 years are the fastest-growing age group among U.S. residents and will reach approximately 8.9 million in 2030. Although the rate of deaths from falls is increasing among all persons aged =65 years, it is increasing fastest among those aged 85 and over (3.9 percent per year). Nationally, the rate of deaths from falls might be increasing because of longer survival after the onset of common diseases such as heart disease, cancer and stroke.
If the current rate remains stable, an estimated 43,000 U.S. residents aged =65 years will die because of a fall in 2030, and if the rate continues to increase, 59,000 fall-related deaths could result.
For more information https://www.cdc.gov/mmwr/volumes/67/wr/mm6718a1.htm?s_cid=mm6718a1
Deaths from falls among persons aged =65 years — United States, 2007–2016
| Characteristic | 2007 | 2016 | 2007–2016 | ||
| No. of deaths | Deaths per 100,000 | No. of deaths | Deaths per 100,000 | Annual percentage change |
|
| Total | 18,334 | 47 | 29,668 | 61.6 | 3.0 |
| Sex | |||||
| Men | 8,408 | 57.9 (56.7–59.2) | 13,721 | 72.3 (71.1–73.5) | 2.4 |
| Women | 9,926 | 40.2 (39.4–41.0) | 15,947 | 54.0 (53.1–54.8) | 3.8 |
| Age group (yrs) | |||||
| 65–74 | 2,594 | 13.2 (12.7–13.7) | 4,479 | 15.6 (15.2–16.1) | 1.8 |
| 75–85 | 6,552 | 50.1 (48.9–51.3) | 8,735 | 61.4 (60.1–62.7) | 2.3 |
| =85 | 9,188 | 182.3 (178.6–186.0) | 16,454 | 257.9 (253.9–261.8) | 3.9 |
Exercise can help prevent falls
Exercise can have a moderate impact on preventing falls in older adults at increased risk for falls, according to the United States Preventive Services Task Force in its final recommendations issued this spring. In many respects, its findings echo those that USPSTF – which is independent of the U.S. government – made in 2012.
USPSTF bases its recommendations on the evidence of both the benefits and harms of specific preventive care services. It does not consider the costs of providing a service in this assessment.
Falls are the leading cause of injury-related morbidity and mortality among older adults in the United States, says USPSTF. In 2014, 28.7 percent of community-dwelling adults 65 years or older reported falling, resulting in 29 million falls (37.5 percent of which needed medical treatment or restricted activity for a day or longer) and an estimated 33,000 deaths in 2015.
Unfortunately, no instrument has been clearly identified as accurate and feasible for identifying older adults at increased risk for falls. According to USPSTF, a patient’s history of falls is the most commonly used factor that consistently identifies persons at high risk for falls.
Exercise interventions
Effective exercise interventions include supervised individual and group classes and physical therapy. The most common exercise component in programs reviewed by USPSTF was gait, balance, and functional training (17 trials), followed by resistance training (13 trials), flexibility (eight trials), and endurance training (five trials). Three studies included tai chi, and five studies included general physical activity. The most common frequency and duration for exercise interventions was three sessions per week for 12 months, although duration of exercise interventions ranged from two to 42 months.
The 2008 U.S. Department of Health and Human Services guidelines recommended that older adults get at least 150 minutes per week of moderate-intensity or 75 minutes per week of vigorous-intensity aerobic physical activity, as well as muscle-strengthening activities twice per week. It also recommended performing balance training on three or more days per week for older adults at risk for falls because of a recent fall or difficulty walking.
In its findings, the USPSTF notes that the National Institute on Aging outlines four interventions for the prevention of falls: exercise for strength and balance, monitoring for environmental hazards, regular medical care to ensure optimized hearing and vision, and medication management. According to the AGS, detecting a history of falls is fundamental to a falls reduction program, and it recommends that all older adults be asked about falls once a year.
The AGS further recommends that older persons who have experienced a fall should have their gait and balance assessed using one of the available evaluations; those who cannot perform or perform poorly should be given a falls risk assessment that includes a focused medical history, physical examination, functional assessment, and an environmental assessment. The AGS also recommends the following interventions for falls prevention:
- Adaptation or modification of home environment (e.g., elimination of clutter and throw rugs, adequate lighting, etc.).
- Withdrawal or minimization of psychoactive or other medications.
- Management of postural hypotension (low blood pressure occurring when standing up from a sitting or lying-down position).
- Management of foot problems and footwear.
- Exercise (particularly balance), strength, and gait training.
- Vitamin D supplementation of at least 800 IU per day for persons with vitamin D deficiency or who are at increased risk for falls.
Source: U.S. Preventive Services Task Force, https://www.uspreventiveservicestaskforce.org/Page/Document/RecommendationStatementFinal/falls-prevention-in-older-adults-interventions1
Home care and safety: A difficult match
Institute for Healthcare Improvement report lists risks, solutions
The safety of care provided in the home has not yet received nearly as much attention as patient safety in hospitals and other clinical settings, despite the fact that the home has become the site of care for many people, says the Institute for Healthcare Improvement (IHI) in its report, “No Place Like Home: Advancing the Safety of Care in the Home.”
In 2016, more than 2 million personal care attendants provided care in the home, according to the U.S. Department of Labor. Across the country, workers from home health agencies provide home health care services to more than 3 million Medicare beneficiaries. The Department of Labor predicts that by 2026, the number of personal care attendants will rise by 40 percent.
IHI convened an expert panel in November 2017 to consider the challenges to safety in the home setting and to offer recommendations for improvement. Its report identifies nine risks and their potential harms:
- Adverse events related to medication and other forms of treatment.
- Injuries due to physical hazards in the home (e.g., falls).
- Injuries related to equipment and technology.
- Pressure injuries.
- Infections.
- Conditions related to poor nutrition.
- Adverse effects on family caregivers.
- Adverse effects on home care workers.
- Potential neglect and abuse of care recipients.
To read more, visit ihi.org/no-place-like-home.