January 10, 2022 – Will the last person not infected with the Covid19 virus please raise their hand?
Of course, the question is facetious – we still know several people fortunate to have avoided infection to this point. But those numbers have dwindled significantly lately.
Reported infections in the United States swelled last week, shattering records set during the Delta wave and the prior pandemic peak last January. Omicron infected 4x as many people last week, compared to the Delta peak at the end of the summer. Compared to the January 11, 2021 pandemic peak, the U.S. reported 2.5x more new cases last week.
Moreover, we know that most new infections go unreported. The test-positive rate is now 5x higher than it was pre-Omicron and rising. The rate is running at 27%. Public health officials believe that a rate above 5% indicates that our testing surveillance fails to measure the full extent of infections.
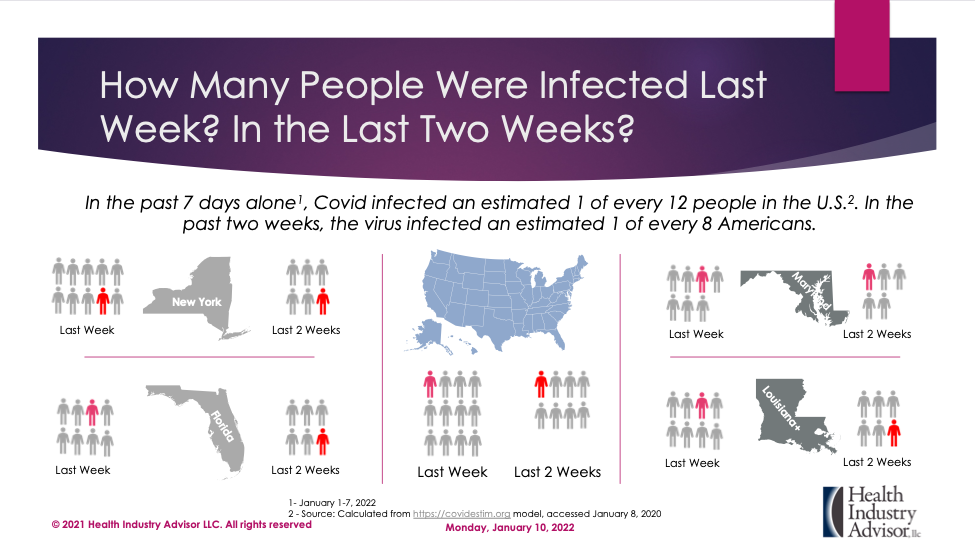
So, how many persons were infected last week? The latest update from the Institute for Health Metrics and Evaluation (IHME) model postulates that 6 million people were infected last Friday alone. A model developed by public health scientists from Harvard, Stanford, and Yale Universities estimates that one in twelve of us were infected last week. The rate jumped to one in eight over the past two weeks.
Sure, infections are rising, but they are generally mild, right? That seems to be true. However, our health system is overwhelmed, and the situation is worsening. In the middle of last week, the average daily census of Covid patients approached record highs. IHME predicts hospitals will fill 50% more beds with Covid patients before this census peaks in late January. Worse, it’s not simply a matter of adding temporary capacity or converting a hospital wing to Covid care. The greatest threat to our health system is finding sufficient caregivers – a challenge only made worse by the exploding infection rate.
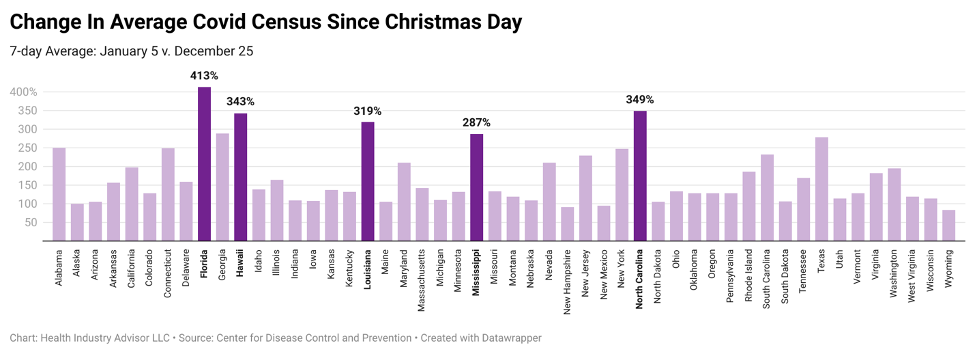
Hospitals in the industrial Northeast and Midwest face the most significant challenges, considering the number of beds devoted to Covid care and the rate of hospitalizations per capita. Nonetheless, the strain on health care resources cuts across the country. Florida posted a fourfold spike in Covid patients since Christmas. This census doubled (at least) during this period in every state except New Hampshire and New Mexico.
The Omicron variant changed the game. This situation is no longer a “pandemic of the unvaccinated,” as the President and federal health officials previously proclaimed. The sheer number of breakthrough infections of vaccinated persons crushes that view.
Still, vaccines deliver robust protection against severe infection: Through October, unvaccinated persons faced a 5x more significant risk of infection and a 14x greater risk of dying than fully vaccinated persons (Centers for Disease Control and Prevention). More recently, New York reported that vaccines provided 77% effectiveness in preventing infection and 92% effectiveness in preventing hospitalization. We note that the New York data reflects the Omicron wave that has rocked that state.
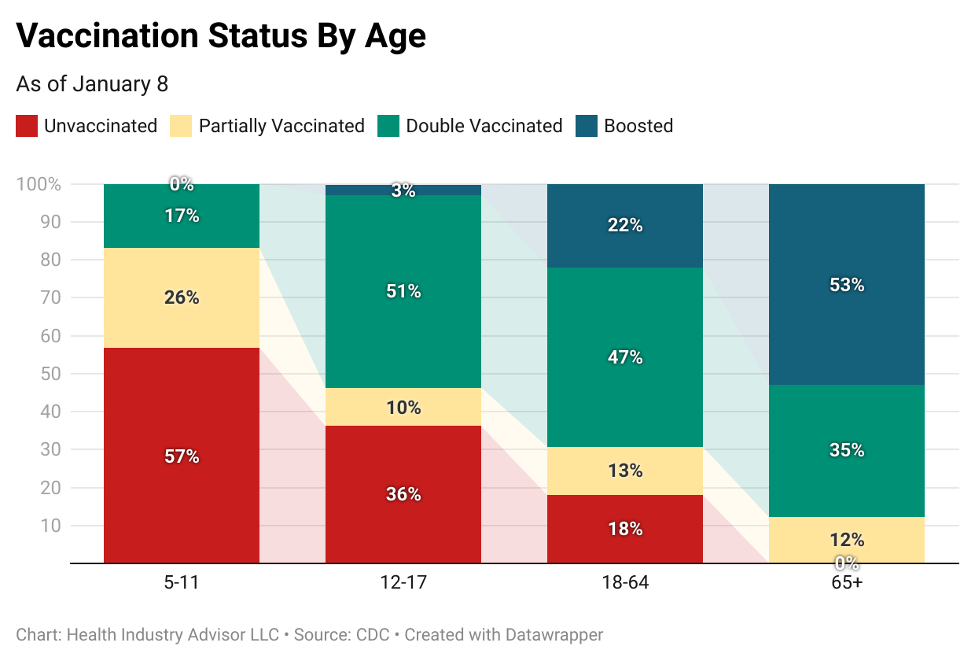
Unfortunately, vaccinations in the U.S. lag most of the developed world. Fewer than two-thirds of the U.S. population completed the two-dose vaccination regimen, and barely one-third of those sought a booster shot. Among working-age adults, nearly one-third have received a single dose or none. Only one in five are boosted.
So, right or wrong, much of the country relies on natural immunity for protection. This strategy carries inherent personal risk (and risk to others) and increases the strain on the health care system. Nevertheless, we cannot ignore natural immunity’s contribution to ending this pandemic.
In overhauling its Covid projection model last month, IHME acknowledged natural immunity’s impact. IHME’s model revision incorporates both Omicron’s rapid transmission and the ongoing vaccination hesitancy in the U.S.
IHME’s latest update (published Saturday) provides a “light at the end of the tunnel” perspective. Indeed, this model conceives those new infections had peaked in the U.S. on Saturday and will peak globally by mid-week. This forecast provides a much rosier outlook than UHME’s previous model, posted December 18. In that forecast, IHME envisioned U.S. infections would not peak until late January.
Daily new infections plunge quickly in IHME’s estimate. Within two weeks, Omicron infects half as many people each day as today. In another two weeks, the daily rate falls by one-half again.
The separate ensemble forecast anticipates cases peaking within the next week or two.
Let’s hope that IHME (and the ensemble forecasters) have it right – that Covid infections are peaking in the United States. Still, the next several weeks pose significant challenges to our health care system: In the IHME model, the Covid census surges for another two weeks. With flu season peaking in the next few weeks as well, patients with respiratory illnesses could overwhelm an already overworked staff.
By Mark Van Sumeren
